CASE REPORT | https://doi.org/10.5005/jp-journals-10015-1865 |
Facial Asymmetry due to Hemifacial Microsomia Managed by an Interdisciplinary Approach: A Case Report
1,5,6Department of Oral and Maxillofacial Surgery, Karpaga Vinayaga Institute of Dental Sciences, Chinna Kolambakkam, Palayanoor, Madurantakam, Tamil Nadu, India
2Department of Orthodontics and Dentofacial Orthopedics, Adhiparasakthi Dental College and Hospital, Melmaruvathur, Tamil Nadu, India
3Department of Conservative Dentistry and Endodontics, Karpaga Vinayaga Institute of Dental Sciences, Chinna Kolambakkam, Palayanoor, Madurantakam, Tamil Nadu, India
4Department of Oral Medicine and Radiology, Karpaga Vinayaga Institute of Dental Sciences, Chinna Kolambakkam, Palayanoor, Madurantakam, Tamil Nadu, India
7Department of Plastic Surgery, Desire Esthetics, Anna Nagar, Chennai, Tamil Nadu, India
Corresponding Author: Balaguhan Balasubramanian, Department of Oral and Maxillofacial Surgery, Karpaga Vinayaga Institute of Dental Sciences, Chinna Kolambakkam, Palayanoor, Madurantakam, Tamil Nadu, India, Phone: +91 9841263109, e-mail: dr.guhan@gmail.com
How to cite this article Balasubramanian B, Venkatachalapathy S, Natarajan K, et al. Facial Asymmetry due to Hemifacial Microsomia Managed by an Interdisciplinary Approach: A Case Report. World J Dent 2021;12(5):427–432.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Aim and objective: The aim of this case report is on an interdisciplinary orthodontic and surgical treatment approach of facial asymmetry due to congenital hemifacial microsomia (HFM).
Background: Hemifacial microsomia is the second common congenital craniofacial deformity after cleft lip and palate, which presents with different clinical characteristics, including an extremely variable asymmetrical presentation. And there is no standardized treatment protocol for this type of asymmetry hence individualized treatment plan for every patient can result in the best esthetic and functional stability.
Case description: This case study emphasizes on an adult patient who has congenital HFM with class I skeletal malocclusion involving asymmetry from the supraorbital level to the lower border of the face. Pre-surgical orthodontics is done initially by aligning the teeth and placing asymmetrical bite block, followed by LeFort I osteotomy with differential impaction (transverse) and bilateral sagittal split osteotomy with rotation along with advancement genioplasty, and finally, post-orthodontic settling done.
Conclusion: A team effort of surgical orthodontists and surgeons with the aid of advanced imaging and software technology made us make an amazing change in patient’s life both esthetically and functionally.
Clinical significance: This new innovative method is both a time-saving and conservative method both for patients and dentists.
Keywords: Advancement genioplasty, Bilateral sagittal split osteotomy, Hemifacial microsomia and LeFort I osteotomy.
BACKGROUND
Hemifacial microsomia (HFM) is a congenital complex malformation syndrome with varied nomenclature with a large host of genetic and embryotoxic associations. The occurrence ranges from 1 in 3,500 to 1 in 5,000 live births, with 3:2 male predominance. The exact etiology of HFM is always varying. Pathogenesis involves in disturbed development of first and second branchial arches, which led to underdevelopment of the temporomandibular joint, mandibular ramus, masticatory muscles, ears, and sometimes it affects facial nerves and muscles.1 A wide spectrum of clinical features was involved like the facial skeleton, muscle, and other organs. Hemifacial microsomia is associated with a deficiency of hard and soft tissues on one side of the face.2
Hemifacial microsomia varies from a minor asymmetry to severe under-development of the semi-facial side along with orbital implications. In certain patients, there will be partial or even a total absence of the ear. Chin and facial midline have eccentrically deviated to the affected side. Commonly one corner of the mouth is situated higher than the other side and result in the rise of the oblique lip line. Sometimes, asymmetry is also associated with unilateral hypoplasty of maxillary bones, temporal, zygomatic arch, and malformations of both external and internal parts of the ear.3
There are various clinical manifestations for this disorder and many classifications and the scoring system have been developed to help and categorize these patients. Véliz et al. in 2016 has summarized all the classifications (Fig. 1).4 One of the classifications that are commonly followed is the classification system of Pruzansky, Pruzansky’s classification modified by Kaban and OMENS. The treatment modality has two approaches–the early and late approaches. In the early (growth phase), conventional surgery by an autologous costochondral bone graft or distraction osteogenesis can be done. While in the late (after the active growth phase), conventional Bi-jaw surgery or bimaxillary distraction osteogenesis was advised.5
Hemifacial microsomia is always associated with deviation of facial bone and malocclusion of dentition. These two changes cannot be corrected by either orthodontic or surgical alone. Hence, the sugico-orthodontic approach is necessary to bring both the esthetic facial smile and good functional occlusion in the patients. Among this classification, this patient comes under class IIA of Pruzansky’s classification modified Kaban. So, we have planned for orthodontic and Bi-jaw surgery along with genioplasty to correct the esthetics and functional problem.
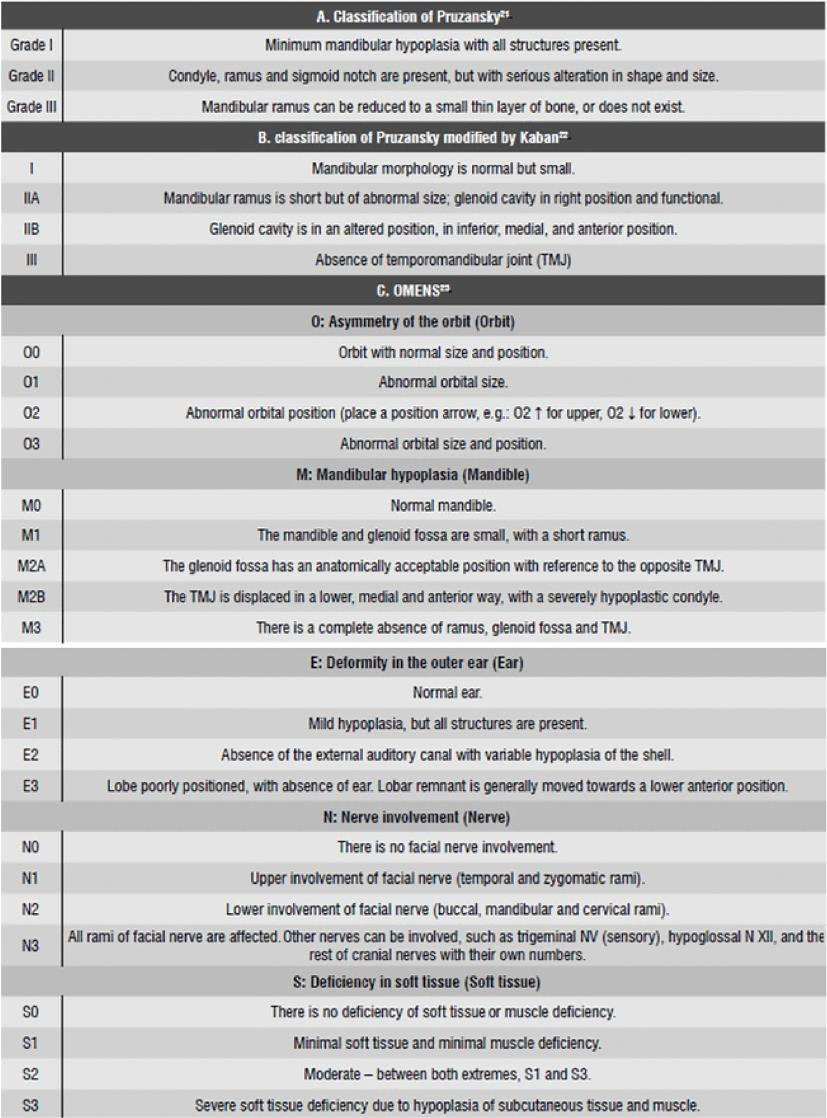
Fig. 1: Various types of clinical features and their classification4

Figs 2A to D: Intraoral occlusion from pre- to post-treatment: (A) Pre-orthodontic occlusion; (B) Pre-surgical occlusion; (C) Immediate postsurgical occlusion; (D) Post-orthodontic occlusion
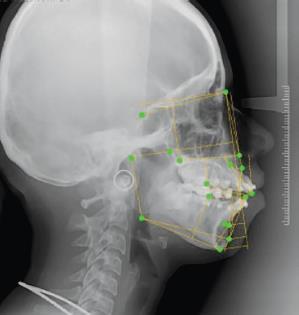
Fig. 3: Pre-surgical lateral cephalogram
CASE DESCRIPTION
A 20-year-old adult female patient visited the Department of Oral and Maxillofacial Surgery, Karpaga Vinayaga Institute of Dental Sciences, with a chief complaint of observable facial asymmetry, difficulty in phonetics, and mastication. The patient was a full-term-born and vaginal born with no significant prenatal, parental, and sibling history. The patient was moderately built, well-nourished, and psychologically stable. Initially, the patient has noticed the deviation of the jaw during smiling from the age of 14 years, and as the growth occurs the deviation becomes more prominent and noticeable.
On extraoral examination, facial asymmetry was there on the right side of the patient from the supraorbital region to the chin. Alar base of the nose and corner of the mouth were at higher level towards the right side. The eyebrow and eye were slightly at a higher level but not noticeable. Chin was shifted toward the right side by 6 mm at rest, which deviated further on mouth opening. At rest, there is no lip incompetency. Muscles of mastication seem to be normal.
On intraoral examination, the patient had class I molar and Kartz class I premolar relationship with crowded upper and lower anterior, highly placed 23 and 33 with a deviation of mandibular midline toward right side by 5 mm associated with severe occlusal canting in transverse dimension. Class I restoration was done in 16, 17, 36, 37, 46, and 47 (Fig. 2A).
Lateral cephalographic evaluation revealed a skeletal class II malocclusion with increased midfacial height associated with retrusive mandible rotated in a clockwise direction, high mandibular plane angle, and deficient chin (Fig. 3). The 3D evaluation of computed tomography (CT) shows asymmetry between zygoma, maxilla, and mandible (Fig. 4).
Analysis of OPG disclosed a prominent anti-gonial notch, irregular shape of head and neck of the condyle, comparatively short ramus on the right side of the mandible, and 5 mm deviation of chin toward the right side. The was diagnosed as HFM (right) on a class I skeletal base, retrusive mandible, high mandibular plane angle, increased lower anterior facial height associated with crowded upper and lower anterior, transverses asymmetry of the face reflecting on the soft tissue profile with the probable etiology of embryological origin (Fig. 5).
Treatment Plan
The main treatment objectives were to correct the asymmetric convex facial profile, malocclusion, open bite, and chewing difficulty. Non-extraction surgico-orthodontic treatment plan was planned: pre-orthodontics (8 months), followed by surgery (4 days of hospitalization and 2 months of healing period) and post-orthodontics settling (6 months). Overall treatment timing was planned for 16–18 months. Photographic VTO (PA view) of the proposed surgical outcome was discussed with the patient and the treatment plan was finalized. The surgical plan was LeFort I osteotomy differential impaction with superior positioning on the left side and inferior positioning on the right and bilateral sagittal split osteotomy with advancement rotation along with advancement genioplasty. After post-orthodontic settlement, patient has been advised to wear retainers. The pre- and post-treatment values were analyzed using COGS analysis from lateral cephalometries.
Pre-orthodontic Procedure
The first step is to align the teeth and to get 23 and 33 into occlusion. This is achieved by bonding 0.022″ × 0.028″ MBT pre-adjusted edgewise prescription appliance (Minidiamond, Ormco. Inc. Ltd., USA). Initial leveling and aligning were carried out with 0.014″ CuNiTi, 0.016″ × 0.022″ NiTi, 0.017″ × 0.025″ NiTi, and 0.019″ × 0.025″ NiTi followed by 0.019″ × 0.025″ SS for final aligning and leveling of upper and lower anterior and 0.021″ × 0.025″ SS as final surgical stabilizing wires (Fig. 2B).
After 8 months of initial alignment and leveling, as per the surgical plan for achieving ideal correction of transverse cant, composite bite blocks were given in 24, 25, 26, and 27 (for further selective trimming and supra-eruption of the left posterior teeth). The upper and lower arch impressions and pre-surgical records were taken. The models were articulated in the Hanau articulator and face bow transfer was done with a spring bow. The mock surgery was done using the Erikson platform and surgical splints were fabricated (Fig. 6). The first primary splint was fabricated after repositioning the maxillary cast then the final splint was done after the advancement rotation of the mandibular cast and the treatment plan was analyzed using NemoCeph Software. After finishing pre-orthodontic procedures, surgery was planned.
Surgical Procedure
Maxillary LeFort I osteotomy was done by considering the Roll axis as a fulcrum. Down grafting on the right side by 3 mm and superior repositioning by 6 mm on the left side was done. A bilateral sagittal split osteotomy (BSSO) cut was made, and the mandibular rotation was done on the pitch axis by 4 mm by maintaining a posterior open bite of 5 mm with the guide of the prefabricated splints. Finally sliding and advancement genioplasty of 5 mm was done. Rigid fixation was done with plates and screws (KLS MARTIN, Tuttlingen, Germany) on both jaws. The patient was hospitalized for 4 days, and a review was done after 8 weeks (Fig. 7).

Fig. 4: Pre-surgical computed tomography (PNS view)

Fig. 5: Pre-surgical OPG

Fig. 6: Model surgery and surgical splint fabrication

Figs 7A to G: Intraoperative surgical procedures. (A) LeFort I osteotomy cut; (B) BSSO rotation; (C) Advancement genioplasty; (D) Intermediate splint in position; (E) Final splint in position; (F and G) Intraoperative left and right occlusion
Post-orthodontic Procedure
After a satisfactory healing, orthodontic treatment was resumed again with heavier 0.021″ × 0.025″ SS wires were replaced with a smaller dimension 0.016″ × 0.022″ TMA in the upper arch and 0.016″ SS round wire in the lower arch. Final finishing and detailing were carried by selectively trimming composite bite block on the left side at an average of 1 mm per month. This resulted in supra-eruption of 24, 25, 26 and 27, and fine-tuning of the transverse occlusal plane. This was accomplished by 3.5 OZ settling elastics (Fig. 2C). Once the settling was completed, the orthodontic appliance was debonded, and removable retainers were given (Fig. 2D).
A 3-year follow-up was done, and the patient has no complaint regarding TMJ, occlusion, speech, and masticatory function. Good stability was maintained, with 3 years of follow-up, which make the patients both esthetically and functionally satisfied.
DISCUSSION
Hemifacial microsomia etiology has been divided based on embryologic, clinical, and laboratory studies. But the pathogenesis is still under mystery. There is a hypothesis that the deficiency in the neural crest of first and second pharyngeal arches results in HFM.5,6 Cousley et al. in 2002 reported that transgenic mutation of B1 to B3 on chromosome 10 in a mouse model was the pathogenesis factor of HFM.7 But the accepted theory was that formation of hemorrhage during embryogenesis, which is associated with the stapedial arterial system, disrupts the normal development of the first and second arch pharyngeal leading to HFM.8 According to laboratory investigations, the early loss of neural crest cells is the main factor, and the amount of loss determines the severity of the facial deficiency and it is genetically inherited.9
The early diagnosis of the patient can be treated in the growth phase. Hemifacial microsomia is not recognizable in an infant due to buccal fat pads and being edentulous. But in the growth phase due to the thinning of buccal fat pads, makes the mandibular deformity to be more obvious during childhood. During the growing phase, the conventional surgical procedure of autologous costochondral bone graft or bimaxillary distraction osteogenesis can be done, depending on individual patients, and considering the pros and cons of these methods. Simultaneous maxillomandibular distraction is the widely accepted one but there is a possibility of injury to the unerupted upper molars. After the growth phase, the bi-maxillary surgical osteotomy is mostly preferred.10
In this paper, we presented a patient with Kaban type IIA (TMJ, ramus and glenoid fossa are hypoplastic, malformed, and malpositioned, but the deformed joint is adequately positioned for the symmetric opening of the mandible) and decided to go for a Bi-jaw surgical procedure which holds advantages like short treatment period, stable clinical and esthetic outcomes as well as cost savings over distraction osteogenesis.
Apart from the regular protocol of Bi-jaw surgery with pre-surgical orthodontics, an innovative procedure of orthodontically—incorporating posterior bite blocks on the normal side allowed the stable position of the splint and the jaw fragments during surgery and transverse canting correction—surgically made this case to be a unique one. Finally, postsurgical orthodontic finishing was performed. In this patient at 0.021″ × 0.025″ SS surgical wire phase, we placed composite posterior bite block on left maxillary buccal teeth for ease of splint fabrication. This aided us in proper positioning of the splint and for semi-rigid internal fixation during surgery. Further postsurgical orthodontic settling was carried out easily by selective trimming of the composite bite block and allowing the supra-eruption of upper left posterior teeth to functional occlusion.
Bailey et al. have done a 5-year follow-up of HFM patients treated with maxillary LeFort I osteotomy combined with sagittal osteotomy of the mandible and concluded that assured long-term stability was achieved except that maxilla has undergone some sagittal displacement in class III and vertical displacements in class II of 1–2 mm, in a negligible number of patients within a duration of 12–18 months after surgery.11 Hence, we opted for Bi-jaw surgery to correct the transverse canting and rigid fixation was done. A 3-year follow-up was done to check for stability and the patient has no complaint. The pre- and post-treatment values confirm that there is good esthetics and functional change in the occlusion (Table 1).
| Parameter | Pre-op | Post-op | Normal value |
|---|---|---|---|
| Cranial base | |||
| ArN (mm) | 78.7 | 78.8 | 88.9 ± 4.1 |
| ArPtm (mm) | 36.6 | 36.6 | 37.1 ± 2.8 |
| PtmN (mm) | 42.1 | 42.1 | 52.8 ± 4.1 |
| Horizontal | |||
| N-A-Pog (degree) | 24.4 | 14.3 | 3.9 ± 6.4 |
| N to A || HP (mm) | 8.1 | 4.3 | 0.0 ± 3.7 |
| N to B || HP (mm) | -1.3 | 0.9 | −5.3 ± 6.7 |
| N to Pg || HP (mm) | -6.3 | 2.5 | −4.3 ± 8.5 |
| Vertical | |||
| N to ANS _|_ HP (mm) | 44.1 | 47 | 54.7 ± 3.2 |
| ANS-Gn _|_ HP (mm) | 42.5 | 54 | 68.6 ± 3.8 |
| N to PNS _|_ HP (mm) | 43.5 | 46 | 53.9 ± 1.7 |
| MP to HP (degree) | 87.9 | 24 | 23 ± 5.9 |
| Upper 1 to NF (mm) | 28.0 | 29 | 30.5 ± 2.1 |
| Lower 1 to MP (mm) | 75.4 | 41 | 45 ± 2.1 |
| Upper 6 to NF (mm) | 26.5 | 25.8 | 26.2 ± 2.0 |
| Lower 6 to MP (mm) | 48.8 | 33.4 | 54.7 ± 3.2 |
| Maxillomandibular | |||
| PNS to ANS || HP (mm) | 40.1 | 43.2 | 57.7 ± 2.5 |
| Go-Pog (mm) | 62.8 | 39.6 | 83.7 ± 4.7 |
| B-Pog || MP (mm) | 16.9 | 17.8 | 8.9 ± 1.7 |
| Ar-Go-Gn (degree) | 193.3 | 116 | 119.1 ± 6.5 |
| Skeletal and dental | |||
| Ramus height (Ar-Go) (mm) | 47.9 | 51.5 | 44 ± 5 |
| Upper OP to HP (degree) | 3.4 | 4.4 | 6.2 ± 5.1 |
| Lower OP to MP (degree) | 6.3 | 5.6 | 6.2 ± 5.1 |
| AB on OP (Wit?) (mm) | 6.8 | 3.1 | −1.1 ± 2.0 |
| Upper 1 to NF angle (degree) | 122.0 | 114 | 111.0 ± 4.7 |
| Lower 1 to MP angle (degree) | 48.1 | 97 | 95.9 ± 65.2 |
CONCLUSION
Presentation of HFM may vary for every individual. Every aspect of the individual and their expectations should have been listened to carefully. There should be good coordination between the patient, surgeon, and orthodontist. The patient should be informed about the outcome of the result after the treatment and about the extent of fulfilment that can be achieved from their expectation. The long-term success of the treatment was attained by a successful interdisciplinary approach. Further facial soft tissue augmentation procedures were advised to the patient for future fine-tuning.
CLINICAL SIGNIFICANCE
In this case, we have made an innovative method of treating HFM, orthodontically by placing an asymmetrical bite block and surgically doing a transverse canting correction, thereby this method will be a simple, conservative, and time-consuming method for both orthodontist and surgeon.
CONSENT OF PATIENT
Consent has been obtained from the patient for publication without revealing her identity.
REFERENCES
1. Cohen MM, Rollnick BR, Kaye CI. Oculoauriculovertebral spectrum: an updated critique. Cleft Palate J 1989;26(4):276–286.
2. Dhillon M, Mohan RPS, Suma GN, et al. Hemifacial microsomia: a clinicoradiological report of three cases. J Oral Sci 2010;52(2):319–324. DOI: 10.2334/josnusd.52.319.
3. Moulin-Romsée C, Verdonck A, Schoenaers J, et al. Treatment of hemifacial microsomia in a growing child: the importance of co-operation between the orthodontist and the maxillofacial surgeon. J Orthod 2004;31(3):190–200. DOI: 10.1179/146531204225022407.
4. Véliz MS, Agurto VP, Leiva VN. Hemifacial microsomia: a literature review. Rev Fac Odontol Univ Antioq 2016;27(2):404–424. DOI: 10.17533/udea.rfo.v27n2a9.
5. Johnson JM, Moonis G, Green GE, et al. Syndromes of the first and second branchial arches, part 1: embryology and characteristic defects. AJNR Am J Neuroradiol 2011;32(1):14–19. DOI: 10.3174/ajnr.A2072.
6. Rahbar R, Robson CD, Mulliken JB, et al. Craniofacial, temporal bone, and audiologic abnormalities in the spectrum of hemifacial microsomia. Arch Otolaryngol Head Neck Surg 2001;127(3):265. DOI: 10.1001/archotol.127.3.265.
7. Cousley R, Naora H, Yokoyama M, et al. Validity of the HFM transgenic mouse as a model for hemifacial microsomia. Cleft Palate-Craniofac J 2002;39(1):81–92. DOI: 10.1597/1545-1569_2002_039_0081_vothtm_2.0.co_2.
8. Poswillo D. The pathogenesis of the first and second branchial arch syndrome. Oral Surgery, Oral Medicine, Oral Pathology 1973;35(3):302–328. DOI: 10.1016/0030-4220(73)90070-4.
9. Naora H, Kimura M, Otani H, et al. Transgenic mouse model of hemifacial microsomia: cloning and characterization of insertional mutation region on chromosome 10. Genomics 1994;23(3):515–519. DOI: 10.1006/geno.1994.1537.
10. Paul MA, Opyrchał J, Knakiewicz M, et al. Hemifacial microsomia review: recent advancements in understanding the disease. J Craniofac Surg 2020;31(8):2123–2127. DOI: 10.1097/SCS.0000000000006616.
11. Bailey LJ, Phillips C, Proffit WR, et al. Five-year follow-up of Le Fort I osteotomies. Int J Adult Orthodon Orthognath Surg 1994;9(3):163–173.
________________________
© The Author(s). 2021 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.