SHORT COMMUNICATION | https://doi.org/10.5005/jp-journals-10015-1719 |
Suture Granuloma in Oral Biopsy Specimen
1–3Department of Oral Pathology and Microbiology, Dr DY Patil Dental College and Hospital, Dr DY Patil Vidyapeeth, Pimpri, Pune, Maharashtra, India
4,5Department of Maxillofacial Surgery and Diagnostic Sciences, Division of Oral Pathology, College of Dentistry, Jazan University, Jazan, Kingdom of Saudi Arabia
Corresponding Author: Sachin C Sarode, Department of Oral Pathology and Microbiology, Dr DY Patil Dental College and Hospital, Dr DY Patil Vidyapeeth, Pimpri, Pune, Maharashtra, India, Phone: +91 9922491465, e-mail: drsachinsarode@gmail.com
How to cite this article Sarode SC, Sarode GS, Sengupta N, et al. Suture Granuloma in Oral Biopsy Specimen. World J Dent 2020;11(2):161–163.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Aim: To give perspective on suture granuloma in oral biopsy specimens.
Background: Suture granuloma is an uncommon finding in the oral biopsy specimens. Suture granulomas may give the impression of both benign and malignant lesions, thus posing a serious diagnostic challenge. Hence, it is very important that oral pathologists should understand pathogenesis and histopathology of this rare phenomenon.
Results: Suture granuloma evokes immunological reaction with recruitment of monocyte macrophages, which ultimately forms epithelioid cells and giant cells. The pathogenetic events were driven by the factors such as interleukins, MHC class II molecules, CD4+ Th1 lymphocytes, transforming and platelet derived growth factors. Histopathologically, they are easy to identify due to characteristic appearance of granuloma surrounding the suture material.
Conclusion: This paper presents a very rare occurrence of suture granuloma in an oral biopsy specimen with special emphasis on pathogenesis and histopathology.
Clinical relevance: Accidental findings in oral pathologies are not very common evidence. Suture granuloma is one such phenomenon that can be mistaken for benign or malignant neoplasm. Hence, it becomes of paramount importance to realize the need of understanding this phenomenon for oral pathologists to avoid diagnostic confusion. This short communication elaborates the histomorphological appearance of suture granuloma, which will help pathologists in accurate diagnosis and hence management.
Keywords: Foreign body reaction, Histopathology, Oral pathology, Suture granuloma.
INTRODUCTION
Granulomas are uncommon disorders characterized by active cell-mediated hypersensitivity due to presence of persistent nondegradable entity and is always associated with focal compact collection of chronic inflammatory cells, macrophages, and giant cells.1 For establishment of granuloma, there is need for high degree of interactions and interplay between antigenic substance, macrophage activity, Th1 and B cell overactivity, and variety of noncellular biological mediators. As there are various types of granulomas, a skillful clinical and a keen histopathological examination are needed for their accurate management.1
An uncommon complication of surgery is the development of postoperative granuloma.2 The etiology of these granulomas is not definite. These foreign body granulomas are nodular lesions, which contain granulation tissue and develop in response to various kinds of foreign bodies such as drugs, artificial substances, as well as chronic bacterial infections.3 Particle materials used in tattoos and cosmetic fillers may also lead to the development of foreign body granulomas.4
An artificial substance like the surgical suture material often leads to the development of granulomas. Suture granuloma is a mass of granulation tissue that usually develops around the infectious agent-associated nidus and is associated with the nonabsorbable suture material. The most commonly involved suture material is silk and rarely can be seen in absorbable and monofilament sutures.2,3,5 Silk is favored because it is cheap, straightforwardly sterilized, responds less with the human tissues, and provides strong wound closure.5 Suture granulomas may give the impression of both benign and malignant lesions, thus posing a serious diagnostic challenge.6
HISTOPATHOLOGY OF SUTURE GRANULOMA
A reaction of some immune cells to a foreign body, in particular an immunoreaction of macrophages, has been noted to develop these granulomas.3 It is a chronic process involving the formation of multinucleated giant cells.7 Histopathologically, suture granulomas are associated with multinucleated giant cells, histiocytes, epithelioid cells, lymphocytes, neutrophils, and eosinophils.4 These cells usually encase the suture material in the form of granuloma formation (Fig. 1). The suture material appears as multiple small round clear bodies with a thin eosinophilic rim arranged in a circular fashion. The multinucleated giant cells contain many nuclei, which are scattered irregularly throughout the cytoplasm (Fig. 1). The formation of granuloma and giant cells can be divided into two steps, which involve the first reaction of the tissue imposed by the passage of the suture needle and specific inflammatory reaction to the suture material.5,7 The foreign body suture material can be detected at the center of the granulomatous lesion under polarized microscopy and it is surrounded by macrophages/monocytes and giant cells.5 Fluorescent microscopy is helpful in identifying the suture material in the histological section. Intriguingly, there is no need for the special stain to distinguish the suture material under a fluorescent microscope as even hematoxylin and eosin stain also produce appreciable excitation. Hematoxylin- and eosin-stained slides visualized with the green excitation filter of a fluorescent microscope show a mass of green fluorescent circular to oval bodies (depending on the cut section) with bright peripheral borders (Fig. 2). As per the available literature, apart from the aforementioned methodology, there are no well-documented methodologies on use of special stain for detection of the suture material in the histopathological section.
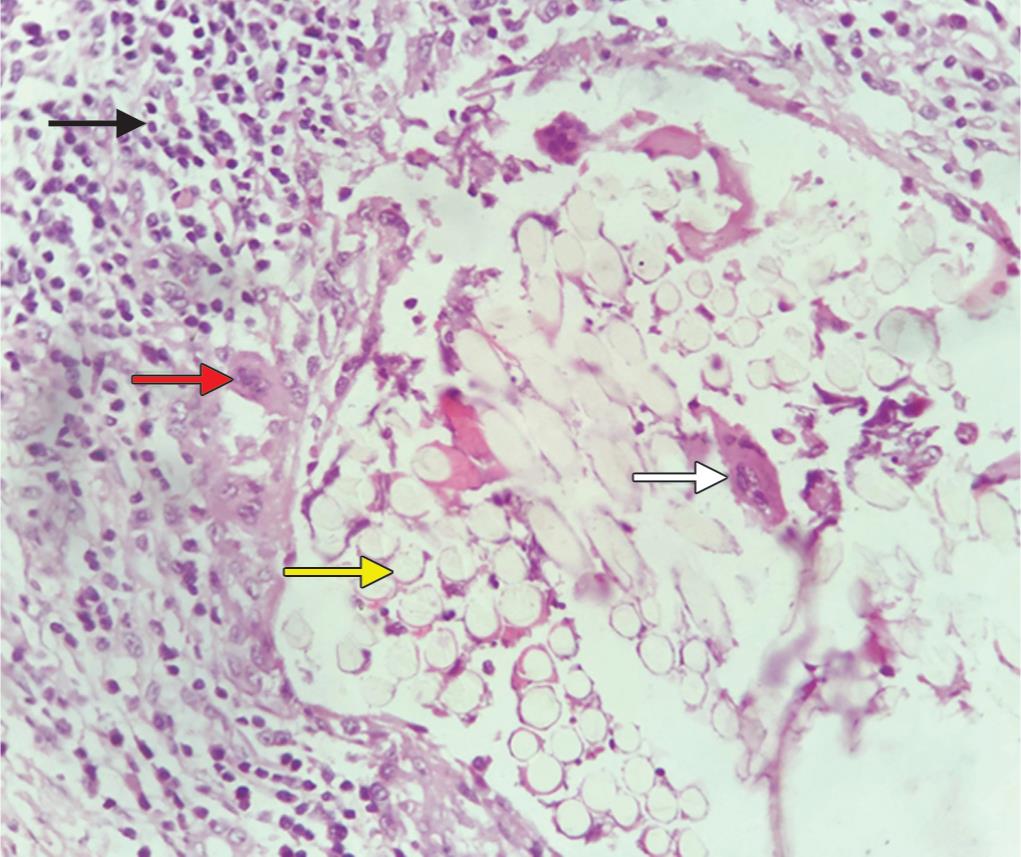
Fig. 1: Photomicrograph showing granuloma formation surrounding the suture material. Granuloma shows mononuclear inflammatory cells (black arrow) and multinucleated giant cells (red arrow). The suture material is characterized by round faint eosinophilic bodies with dark eosinophilic rim (yellow arrow). Some giant cells were seen engulfing the suture material (total magnification X400; hematoxylin and eosin stain)
PATHOGENESIS
The suture material present in the tissue acts as a foreign material and evokes immunological reaction with recruitment of monocyte macrophages, which ultimately forms epithelioid cells and giant cells.8
As the disease progresses, granuloma becomes an active site for numerous enzymes and cytokines. Among these, the most common are the activated macrophages with increased expression of major histocompatibility complex (MHC) class II molecules. These molecules then attract CD4+ Th1 lymphocytes in the granuloma site.8,9 The T helper cells play a major role by recognizing the protein peptide (antigen) belonging to the suture material. This then causes the induction of interleukin-1 on resident macrophages, which initiates cavalcade of chemotactic factors to promote granulomagenesis. Moreover, interferon gamma (IFN-γ) upsurges the expression of MHC class II molecules on macrophages. The activated macrophage receptors carry an Fc fraction of IgG that enhances their capacity to engulf the foreign materials such as suture.10 The final outcome of this process is the formation of well-organized epithelioid granuloma, which ultimately progressed toward the transforming—and platelet—derived growth factor driven fibrosis.8–10

Fig. 2: Photomicrograph of the same field (Fig. 1) under a fluorescent microscope (with green excitation filter) showing the suture material with bright intensity. Some of the suture materials are cut in cross-section (white arrow) and others are in longitudinal section (red arrow)
DISCUSSION
Many cases of suture granulomas have been reported to occur after many years of different kinds of surgeries.3 Suture granulomas have been noted in gastrointestinal and thoracic surgeries,3 head and neck surgeries,3 orchiectomy,5,7 thyroidectomy,6,11 eye surgeries.12 and many other surgeries. They are often interpreted as suspicious for recurrent neoplasm. Yoshioka et al.3 reported a case of suture granuloma mimicking tumor recurrence in the field of radiation in a patient who underwent head and neck surgery for oral squamous cell carcinoma. Post-thyroidectomy suture granulomas have also been noted, presenting as a painless, palpable mass in the surgical bed.6,11 Suture granulomas should be regarded as differential diagnosis for nodules occurring after surgery, in addition to tumor reccurence.3 Apart from the recurrent neoplasm, chronic nonspecific granulomatous lesions and fungal or bacterial infections can be considered as differential diagnosis of this phenomenon.
Suture granulomas are extremely uncommon lesion in oral lesion.3 The main reason could be attributed to the smaller biopsy size that does not need suturing. Moreover, repeat biopsy is not needed in the majority of the lesion of the oral pathology. Hence, at the time of repeat biopsy there are less chances of the suture material being present in the biopsy specimen. The presence of suture granuloma in the surgically excised specimen of oral squamous cell carcinoma is more likely. The present case was reported as accidental finding at the surgical margin examination of the excised oral squamous cell carcinoma specimen. Literature search depicts reports of accidental pathologies at surgical margins such as mucocele.13
Appropriate clinical, radiological, and pathological interpretation is highly recommended in cases with suture granuloma. Sonographic evaluation of nodules and fine-needle aspiration cytology are a few basic diagnostic modalities for suture granulomas.5,6,11 The final diagnosis is usually provided by surgical excision of the lesion and its histopathological examination.5 A histopathologist should be well versed with the histomorphological appearance of the so as to arrive at accurate diagnosis. Although suture granulomas are easily identified with the help of routine hematoxylin and eosin staining, special modalities like polarized microscopy and fluorescent microscopy can be used as adjunct diagnostic tools. To the best of our knowledge, the present paper represents the first report of fluorescent microscopic view of suture granuloma in an oral biopsy specimen.
Apart from granuloma formation, the suture can also be involved and associated with local recurrence of malignancy. This phenomenon is called suture line recurrence and is well documented in the literature for various malignancies including oral squamous cell carcinoma.14–18 Some investigators believe that suture line recurrence occurs due to carcinogenic potential of the suture material.18 However, this might not be true but suture line recurrence very closely resembles clinically to conventional suture granuloma. Recently, it was proposed that surface topography of the suture material might change the mechanobiology of tumor cells and thus leads to recurrence long its line.18 Hence, it is recommended that every postoperative suture granuloma should compulsorily be checked carefully for the possible presence of suture line recurrence.
CONCLUSION
To conclude, suture granuloma is a benign tumor-like mass developing at the site of surgery as a result of the foreign body response to the surgical suture and its constituents. It may occur anywhere in the body and rarely in the oral biopsy specimens. We presented a very rare event of presence of suture granuloma at the surgical margins of oral squamous cell carcinoma. The diagnosis of suture granuloma is specifically of great importance in patients treated for cancer, as it resembles local tumor recurrence. Surgical excision of the lesion is recommended to arrive at the final diagnosis and eradicate source of nidus. Suture line recurrence also looks clinically similar to the suture granulomas. Hence, these granulomas must be considered as differential diagnosis of tumor recurrence and managed as early as possible. Detection of postoperative foreign bodies is of great importance to prevent fatal complications. Retrospective studies on oral specimens are recommended to find out missed out suture granulomas. This will possibly give us more accurate incidence rate and other insights.
REFERENCES
1. James DG. A clinicopathological classification of granulomatous disorders. Postgrad Med J 2000;76(898):457–465. DOI: 10.1136/pmj.76.898.457.
2. Lynch TH, Waymont B, Beacock CJ, et al. Paravesical suture granuloma: a problem following herniorrhaphy. J Urol 1992;147(2):460–462. DOI: 10.1016/s0022-5347(17)37273-7.
3. Yoshioka Y, Nakatao H, Hamana T, et al. Suture granulomas developing after the treatment of oral squamous cell carcinoma. Int J Surg Case Rep 2018;50:68–71. DOI: 10.1016/j.ijscr.2018.07.021.
4. Molina-Ruiz AM, Requena L. Foreign body granulomas. Dermatol Clin 2015;33(3):497–523. DOI: 10.1016/j.det.2015.03.014.
5. Secil M, Mungan U, Yorukoglu K. Suture granuloma after orchiectomy: sonography, doppler and elastography features. Int Braz J Urol 2015;41(4):813–816. DOI: 10.1590/S1677-5538.IBJU.2013.0207.
6. Mathai AM, Preetha K, Valsala Devi S, et al. Post-thyroidectomy suture granuloma: a diagnosis on fine needle aspiration cytology. Diagn Cytopathol 2018;46(9):756–759. DOI: 10.1002/dc.23942.
7. Alkan S, Akdeniz R, Sungur M, et al. Silk suture granuloma after high orchiectomy. Urologiia (Moscow, Russia: 1999) 2020(6):113.
8. James DG. What makes granulomas tick? Thorax 1991;46(10):734–736. DOI: 10.1136/thx.46.10.734.
9. James DG. Granuloma formation signifies a Th1 cell profile. Sarcoidosis 1995;12(2):95–97.
10. Roman J, Jeon YJ, Gal A, et al. Distribution of extracellular matrices, matrix receptors, and transforming growth factor-beta 1 in human and experimental lung granulomatous inflammation. Am J Med Sci 1995;309(3):124–133. DOI: 10.1097/00000441-199503000-00002.
11. Aga H, Hirokawa M, Suzuki A, et al. Sonographic evaluation of nodules newly detected in the neck after thyroidectomy: suture granuloma versus recurrent carcinoma. Ultrasound Int Open 2018;4(04):124–130. DOI: 10.1055/a-0749-8688.
12. Mathew AA, Kowal L. Conjunctival granuloma post pulley fixation suture. J AAPOS 2017;21(4):342–343. DOI: 10.1016/j.jaapos.2017.03.012.
13. Sarode GS, Sarode SC. Superficial mucoceles at surgical mucosal margins of excised oral cancer specimens: an unexpected finding. Oral Oncol 2016;56:e1–e2. DOI: 10.1016/j.oraloncology.2015.12.009.
14. Shinohara T, Kashiwagi H, Nakada K, et al. Suture line recurrence in the jejunal pouch after curative proximal gastrectomy for gastric cancer: report of two cases. Hepato-gastroenterology 2007;54(78):1902–1904.
15. Dehni N, Caplin S, Frileux P, et al. Cancer recurrence along the pouch longitudinal suture line after colonic J pouch-anal anastomosis. Br J Surg 2002;89(2):206–207. DOI: 10.1046/j.1365-2168.2002.01992.x.
16. Hsu TC, Chen MJ. Presence of colon carcinoma cells at the resection line may cause recurrence following stapling anastomosis. Asian J Surg 2018;41(6):569–572. DOI: 10.1016/j.asjsur.2018.01.006.
17. Leinhardt DJ, Smart PJ, Howat JM. Jejunal carcinoma associated with non-absorbable suture material. Postgrad Med J 1988;64(755):716–717. DOI: 10.1136/pgmj.64.755.716.
18. Sarode SC, Sarode GS, Patil S. Suture line recurrence and oral squamous cell carcinoma: a viewpoint. Oral Oncol 2020. 104633. DOI: 10.1016/j.oraloncology.2020.104633.
________________________
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.